By Evan M. Gwilliam, DC, MBA, QMCC, CPC, CCPC, CPMA, CPCO, AAPC Fellow
Practisync Senior Vice President
Reimbursement in healthcare is about conveying that a service was done for good reason. When a provider documents the services delivered during a healthcare encounter, the notes should explain what happened and why. Ideally, the entity paying for the services would pick up those notes, and read them over, and then provide the reimbursement. However, that is impractical and time consuming.
Instead, we convert that information into shorthand codes. There are Current Procedural Terminology (CPT) codes for the procedures and International Classification of Disease (ICD-10) codes for the diagnoses. Then we take these codes and we list them on a CMS-1500 claim form. Therefore, the party responsible for payment doesn’t have to read all the notes; rather, they can just take the shorthand codes from the one-page form and hopefully find all the information they need to adjudicate the claim.
Unfortunately, many clinics fail to utilize the claim form to communicate effectively with payers and claims adjusters. The big box, 24, on the bottom half of the form, is where the procedure codes are listed. There is a column in this box that is often overlooked, but it can make a huge difference when it comes to sending out clean claims and having them adjudicated properly.
Column E is the secret. It is here where the provider can convey clinical information that is contained in the notes. This is the “diagnosis pointer” column. It allows the provider to explain the specific reason behind the specific procedure or service listed on that line. There is space for twelve diagnoses in Box 21, but you can only point to the top four diagnoses for each procedure in box 24E.
Many times, problems begin when doctors list a procedure and link it to a diagnosis that doesn’t make sense for that procedure. Thus, when you do not point (or list in box 24E) a diagnosis or diagnoses that directly correlate to the service listed on the same line in box 24D, then a payer has reason to deny that service line.
For example, if the procedure code is 98940 Chiropractic Manipulative Treatment; spinal, 1-2 regions, and the diagnosis pointer in Column E points to M99.06 Segmental and somatic dysfunction of lower extremity, then that seems to indicate that the spinal procedure was done in an area where there is no spine, and that doesn’t add up. Unfortunately, some offices just let their software default point to the first four diagnoses, with no regard for making sure they link to the right ones. And the claims adjustor can look at this and deny claims.
Here is an example from a client who was having trouble with denials and was looking to figure out why. The five diagnosis codes listed in Box 21 are:
- S39.012A – Strain of muscle, fascia and tendon of lower back, initial encounter
- M95.5 – Acquired deformity of pelvis
- M40.03 – Postural kyphosis, cervicothoracic region
- M62.40 – Contracture of muscle, unspecified site
- M99.06 – Segmental and somatic dysfunction of lower extremity
The six procedure codes reported in Box 24D are:
- 99213 – Office or other outpatient visit for the evaluation and management, level 3
- 98941 – Chiropractic manipulative treatment (CMT); spinal, 3-4 regions
- 98943 – Chiropractic manipulative treatment (CMT); extraspinal, 1 or more regions
- 97110 – Therapeutic procedure, 1 or more areas, each 15 minutes; therapeutic exercises to develop strength and endurance, range of motion and flexibility
- 97032 – Application of a modality to 1 or more areas; electrical stimulation (manual), each 15 minutes
- 97012 – Application of a modality to 1 or more areas; traction, mechanical
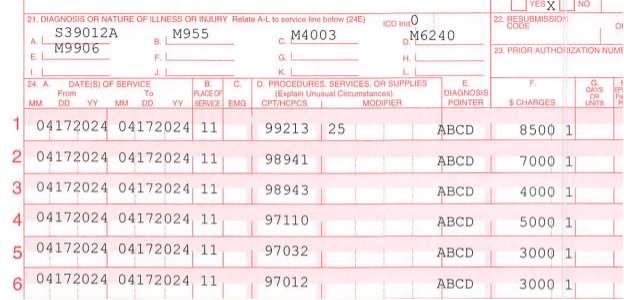
Note that every procedure points to the same four diagnoses in column E. Most likely this is the default for the billing software and no one has bothered to try pointing the diagnoses for each procedure. We’ll look at each procedure code and evaluate the diagnosis pointing for each one.
- 99213: Evaluations are codes that can comfortably point to any and all diagnoses, as any of them can be tied to the delivery of this service.
- 98941: It can be argued that there should be 3-4 diagnoses of segmental dysfunction (subluxation) in order to justify a 3-4 region adjustment. But this code does not point to any diagnoses of segmental dysfunction (M99.0-). The other codes might be considered secondary diagnoses (using Medicare as the standard) to support the need for an adjustment, but only if the provider is trying to indicate that the adjustment can help with those problems.
Clinically it might be argued that manipulation of an area with a muscle strain (box 21 A: S39.012A) might be contraindicated, though. It is probably better to immobilize a tear initially, rather than manipulate it. A deformity of the pelvis (box 21 B: M95.5) is another code that might not support manipulation, although the notes might explain the provider rationale and how they feel the deformity might be impacted by the adjustment. A claims adjuster might deny this code and claim it wasn’t medically necessary for all these reasons.
- 98943: The four diagnoses in box 24E (ABCD) for this extraspinal service are all considered to apply to part of the spinal region; therefore, this procedure is not supported on the claim form. Based on what is available on this list, 98943 should only point to segmental dysfunction of the lower extremity (box 21E: M99.06), which is the only extraspinal diagnosis listed. It would not be a bad idea to have a secondary diagnosis for that lower extremity as well (which is the model outlined by Medicare for spinal manipulation) and could be added here for good measure. This procedure should be denied based on this claim form.
- 97110: While it is possible that the exercises performed by this patient could be designed to directly impact all four of the diagnoses listed in box 24D, it is likely that only one or two of the diagnoses are targeted. For example, stretches might be great for a contracture (box 21D: M62.40). Unfortunately, this is an unlisted code. If used, it means that the provider chose not to document the location of the muscle contracture. There really is no excuse for using unspecified codes when codes with anatomic locations are available. A claims adjuster may deny payment based on this issue alone, because he or she can’t tell where the service was performed.
- 97032: Manual electrical stimulation is a code that is overused often. Most chiropractic physicians do not perform this type of e-stim. They use interferential, or TENS, or maybe Russian stim, which are more correctly billed as 97014 (or G0283 for some payers). The documentation rarely, if ever, supports that the stimulation was actually done manually, such as when the probe is being constantly moved around by the provider throughout the duration of the timed service.
Nonetheless, it does not make sense to point this procedure code to deformity of the pelvis (box 21B: M95.5), though it might be argued that it can affect the muscle strain (box 21A: S39.012A) or the unlisted contracture (box 21D: M62.40). In other words, it ought to only point to one or two diagnoses, not four.
- 97012: Indications for mechanical traction may include neck and back pain, disc injuries, sciatica, and degeneration, so it might be appropriate for diagnoses A, C, or D. However, if the notes are reviewed, they likely indicate that the traction targeted a single body region, but A, C, and D, represent three different parts of the body. If there was some sort of full body traction, then those diagnoses might work, but it might be argued that deformity of the pelvis (box 21 B: M95.5) doesn’t really belong with traction. In fact, that diagnosis code could still be included, but might be last in box 21 and not pointed to by any procedure, which indicates that it complicates the case, but is not being directly managed.
Note that, in 2020, clarification was added to the mechanical traction code to indicate that it is not the correct code to report the use of a roller table, which is common in a chiropractic setting. Rather, 97039, unlisted modality, should be used to report that type of traction.
The moral of this story is this: Document really well and explain everything in the records. Pick diagnoses that support the services the patient needs. Then take the extra few seconds required to point the diagnoses to the appropriate procedures. If a reviewer can’t connect the dots, he or she will need to ask to see the records or may just deny the claim outright. Use the diagnosis pointer column (24E) to your advantage and reduce denials.
Dr. Gwilliam is the Senior Vice President of Practisync, which helps practices improve efficiency and collect more through outsourced expert billing services. As a member of the Kansas Chiropractic Association you can qualify for special rates. If you would like to see if Practisync could be a good fit, reach out to Dr. Gwilliam at evan.gwilliam@practisync.com or visit Practisync.com for more details.